Top of the pageCheck Your Symptoms
Rash, Age 12 and Older
Overview
Rash in teens and adults: Overview
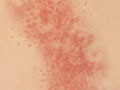
Healthy skin provides a barrier between the inside of the body and the outside environment. A rash means that some change has affected the skin.
In many cases, rashes are caused by skin irritation, which can have many causes. A rash is often a minor problem that may go away with home treatment. But sometimes a rash doesn't go away, or the skin may get so irritated that medical care is needed.
In adults and older children, rashes are often caused by contact with a substance that irritates the skin (contact dermatitis, Opens dialog). Contact dermatitis may cause mild redness of the skin or a rash of small red bumps. A more severe reaction may cause swelling, redness, and larger blisters. The location of the rash may give you a clue about the cause.
Contact dermatitis doesn't always occur the first time you are in contact with the irritating substance (allergen, Opens dialog). After you've had a reaction to the substance, a rash can occur in response to even very small amounts of the substance. Contact dermatitis isn't serious, but it's often very itchy. Common causes include:
- Poisonous plants, such as poison ivy, oak, or sumac, Opens dialog.
- Soaps, detergents, shampoos, perfumes, cosmetics, or lotions.
- Jewelry or fabrics.
- New tools, toys, appliances, or other objects.
- Latex. Allergy to natural rubber latex affects people who are exposed to rubber products on a regular basis. It's often seen in health care workers, rubber industry workers, and people who've had multiple surgeries. Latex allergies can cause a severe reaction.
Rashes may occur with:
- Viral infections, such as herpes zoster, Opens dialog.
- Fungal infections, such as a yeast infection (Candida albicans).
- Bacterial infections, such as impetigo, Opens dialog.
- Sexually transmitted infections (STIs), Opens dialog.
Rashes may also occur as a symptom of a more serious disease, such as liver disease, kidney disease, or some types of cancer.
Rashes may appear after exposure to an insect or a parasite, such as the scabies, Opens dialog mite. You may get a rash when you travel to a rural area or go hiking or camping in the woods.
A rash may be a sign of a chronic skin problem, such as acne, Opens dialog, eczema, Opens dialog, psoriasis, Opens dialog, or seborrheic dermatitis, Opens dialog. Other causes of rashes include dry, cold weather; extremely hot weather (heat rash); and emotional stress.
Some medicines can cause a rash as a side effect. A very rare and serious type of generalized (whole-body) red rash called toxic epidermal necrolysis (TEN). TEN can cause the skin to peel away, leaving large areas of tissue that weep or ooze fluid like a severe burn. TEN may occur after the use of some medicines. If this type of rash occurs, you need to see a doctor.
The need for medical treatment often depends on what other symptoms you have. A rash that occurs with other symptoms, such as shortness of breath or fever, may mean another problem, such as a serious allergic reaction, Opens dialog or infection.
The medical assessment of symptoms is based on the body parts you have.
- If you are transgender or nonbinary, choose the sex that matches the body parts (such as ovaries, testes, prostate, breasts, penis, or vagina) you now have in the area where you are having symptoms.
- If your symptoms aren’t related to those organs, you can choose the gender you identify with.
- If you have some organs of both sexes, you may need to go through this triage tool twice (once as "male" and once as "female"). This will make sure that the tool asks the right questions for you.
Many things can affect how your body responds to a symptom and what kind of care you may need. These include:
- Your age. Babies and older adults tend to get sicker quicker.
- Your overall health. If you have a condition such as diabetes, HIV, cancer, or heart disease, you may need to pay closer attention to certain symptoms and seek care sooner.
- Medicines you take. Certain medicines, such as blood thinners (anticoagulants), medicines that suppress the immune system like steroids or chemotherapy, herbal remedies, or supplements can cause symptoms or make them worse.
- Recent health events, such as surgery or injury. These kinds of events can cause symptoms afterwards or make them more serious.
- Your health habits and lifestyle, such as eating and exercise habits, smoking, alcohol or drug use, sexual history, and travel.
Try Home Treatment
You have answered all the questions. Based on your answers, you may be able to take care of this problem at home.
- Try home treatment to relieve the symptoms.
- Call your doctor if symptoms get worse or you have any concerns (for example, if symptoms are not getting better as you would expect). You may need care sooner.
Sudden tiny red or purple spots or sudden bruising may be early symptoms of a serious illness or bleeding problem. There are two types.
Petechiae (say "puh-TEE-kee-eye"):
- Are tiny, flat red or purple spots in the skin or the lining of the mouth.
- Do not turn white when you press on them.
- Range from the size of a pinpoint to the size of a small pea and do not itch or cause pain.
- May spread over a large area of the body within a few hours.
- Are different than tiny, flat red spots or birthmarks that are present all the time.
Purpura (say "PURR-pyuh-ruh" or "PURR-puh-ruh"):
- Is sudden, severe bruising that occurs for no clear reason.
- May be in one area or all over.
- Is different than the bruising that happens after you bump into something.
If you're not sure if a fever is high, moderate, or mild, think about these issues:
With a high fever:
- You feel very hot.
- It is likely one of the highest fevers you've ever had. High fevers are not that common, especially in adults.
With a moderate fever:
- You feel warm or hot.
- You know you have a fever.
With a mild fever:
- You may feel a little warm.
- You think you might have a fever, but you're not sure.
Temperature varies a little depending on how you measure it. For adults and children age 12 and older, these are the ranges for high, moderate, and mild, according to how you took the temperature.
Oral (by mouth) temperature
- High: 104°F (40°C) and higher
- Moderate: 100.4°F (38°C) to 103.9°F (39.9°C)
- Mild: 100.3°F (37.9°C) and lower
A forehead (temporal) scanner is usually 0.5°F (0.3°C) to 1°F (0.6°C) lower than an oral temperature.
Ear temperature
- High: 105°F (40.6°C) and higher
- Moderate: 101.4°F (38.6°C) to 104.9°F (40.5°C)
- Mild: 101.3°F (38.5°C) and lower
Armpit (axillary) temperature
- High: 103°F (39.5°C) and higher
- Moderate: 99.4°F (37.4°C) to 102.9°F (39.4°C)
- Mild: 99.3°F (37.3°C) and lower
Certain health conditions and medicines weaken the immune system's ability to fight off infection and illness. Some examples in adults are:
- Diseases such as diabetes, cancer, heart disease, and HIV/AIDS.
- Long-term alcohol and drug problems.
- Steroid medicines, which may be used to treat a variety of conditions.
- Chemotherapy and radiation therapy for cancer.
- Other medicines used to treat autoimmune disease.
- Medicines taken after organ transplant.
- Not having a spleen.
Abnormal bleeding means any heavy or frequent bleeding or any bleeding that is not normal for you. Examples of abnormal bleeding include:
- Nosebleeds.
- Vaginal bleeding that is different (heavier, more frequent, at a different time of month) than what you are used to.
- Rectal bleeding and bloody stools.
- Bloody or pink urine.
- Gums that bleed easily when you eat or gently brush your teeth.
When you have abnormal bleeding in one area of your body, it's important to think about whether you have been bleeding anywhere else. This can be a symptom of a more serious health problem.
Symptoms of serious illness may include:
- A severe headache.
- A stiff neck.
- Mental changes, such as feeling confused or much less alert.
- Extreme fatigue (to the point where it's hard for you to function).
- Shaking chills.
Symptoms of infection may include:
- Increased pain, swelling, warmth, or redness in or around the area.
- Red streaks leading from the area.
- Pus draining from the area.
- A fever.
Shock is a life-threatening condition that may quickly occur after a sudden illness or injury.
Adults and older children often have several symptoms of shock. These include:
- Passing out (losing consciousness).
- Feeling very dizzy or lightheaded, like you may pass out.
- Feeling very weak or having trouble standing.
- Not feeling alert or able to think clearly. You may be confused, restless, fearful, or unable to respond to questions.
Many prescription and nonprescription medicines can cause a rash. A few common examples are:
- Antibiotics.
- Aspirin, ibuprofen (Advil, Motrin), and naproxen (Aleve).
- Pain medicines, such as codeine.
- Seizure medicines.
Symptoms of a severe allergic reaction (anaphylaxis) may include:
- The sudden appearance of raised, red areas (hives) all over the body.
- Rapid swelling of the throat, mouth, or tongue.
- Trouble breathing.
- Passing out (losing consciousness). Or you may feel very lightheaded or suddenly feel weak, confused, or restless.
- Severe belly pain, nausea, vomiting, or diarrhea.
A severe reaction can be life-threatening. If you have had a bad allergic reaction to a substance before and are exposed to it again, treat any symptoms as an emergency. Even if the symptoms are mild at first, they may quickly become very severe.
Based on your answers, you may need care soon. The problem probably will not get better without medical care.
- Call your doctor or telehealth provider today to discuss the symptoms and arrange for care.
- If you cannot reach your doctor or telehealth provider or you don't have one, seek care today.
- If it is evening, watch the symptoms and seek care in the morning.
- If the symptoms get worse, seek care sooner.
What are your options for medical care?
Today your options for where to get your medical care are greater than ever before. You may not even have to leave your home to get the care you want and need. You can choose based on what your health problem is and what works best for you.
- Telehealth is a video call with a health care provider. It can be a convenient way to get medical advice or treatment. Some insurers provide access to telehealth that may be available 24 hours a day. Telehealth for less serious problems may cost less and be faster than in-person clinic visits.
- Urgent care and retail clinics are options if you don't have a doctor, you can't or don't want to wait to see your own doctor, or a telehealth visit can’t treat the problem.
- Virtual care from your primary provider or a telehealth service can be delivered through your smartphone, computer, or tablet.
Based on your answers, the problem may not improve without medical care.
- Make an appointment to see your doctor in the next 1 to 2 weeks, or contact your telehealth provider.
- If appropriate, try home treatment while you are waiting for the appointment.
- If symptoms get worse or you have any concerns, call your doctor or telehealth provider. You may need care sooner.
What are your options for medical care?
Today your options for where to get your medical care are greater than ever before. You may not even have to leave your home to get the care you want and need. You can choose based on what your health problem is and what works best for you.
- Telehealth is a video call with a health care provider. It can be a convenient way to get medical advice or treatment. Some insurers provide access to telehealth that may be available 24 hours a day. Telehealth for less serious problems may cost less and be faster than in-person clinic visits.
- Urgent care and retail clinics are options if you don't have a doctor, you can't or don't want to wait to see your own doctor, or a telehealth visit can’t treat the problem.
- Virtual care from your primary provider or a telehealth service can be delivered through your smartphone, computer, or tablet.
Seek Care Now
Based on your answers, you may need care right away. The problem is likely to get worse without medical care.
- Call your doctor now to discuss the symptoms and arrange for care.
- If you cannot reach your doctor or you don't have one, seek care in the next hour.
- You do not need to call an ambulance unless:
- You cannot travel safely either by driving yourself or by having someone else drive you.
- You are in an area where heavy traffic or other problems may slow you down.
Call 911 Now
Based on your answers, you need emergency care.
Call 911 or other emergency services now.
Sometimes people don't want to call 911. They may think that their symptoms aren't serious or that they can just get someone else to drive them. Or they might be concerned about the cost. But based on your answers, the safest and quickest way for you to get the care you need is to call 911 for medical transport to the hospital.
R 14.3.0.0
Most rashes will go away without medical treatment. Home treatment can often relieve pain and itching until the rash goes away.
After a rash appears, leave it alone as much as you can.
- Use soap and water sparingly.
- Leave the rash exposed to the air when you can.
- Don't scratch the rash.
But if you have come in contact with a substance such as poison ivy, oak, or sumac, Opens dialog, wash the area with a lot of water right away. If you can, use liquid dish soap or a mild soap and very warm running water.
If you have a rash, you should not be in contact with children or anyone who is pregnant. Most viral illnesses that cause a rash are contagious, especially if you also have a fever.
Relief from itching
Try these tips to help relieve itching from a rash.
- Keep the itchy area cool and moist.
Put cloths soaked in ice water on the rash a few times a day. Too much wetting and drying will dry the skin, which can increase itching.
- Keep cool, and stay out of the sun.
Heat makes itching worse.
- Add a handful of oatmeal (ground to a powder) to your bath.
Or you can try an oatmeal bath product, such as Aveeno.
- Avoid scratching as much as you can.
Scratching leads to more scratching. Cut nails short or wear cotton gloves at night to prevent scratching.
- Wear cotton clothing.
Don't wear wool and synthetic fabrics next to your skin.
- Use gentle soaps on your skin.
Examples are Basis, Cetaphil, Dove, and Oil of Olay. Use as little soap as you can. Don't use deodorant soaps.
- Wash your clothes with a mild soap, rather than a detergent.
Try using ones like CheerFree or Ecover. Rinse twice to remove all traces of the soap. Don't use strong detergents.
- Don't let the skin get too dry.
Dry skin may make itching worse.
- Try nonprescription medicines for itching.
Carefully read and follow all label directions on the medicine bottle or box.
- Try calamine lotion for a rash caused by contact dermatitis, Opens dialog, such as poison ivy or poison oak rashes.
- For severe itching from contact dermatitis, apply hydrocortisone cream 4 times a day until the itch is gone. But don't use this cream on a fungal rash, because it can make the rash worse.
- If itching affects your sleep, ask your doctor if you can take an antihistamine that might reduce itching and make you sleepy, such as diphenhydramine (Benadryl). Be safe with medicines. Read and follow all instructions on the label.
- Take breaks.
Take several breaks during the day to do a relaxation exercise if stress appears to cause your itching or make it worse. In particular, do it before you go to bed. Sit or lie down, and try to clear your mind. Manage your stress by relaxing every muscle in your body, starting with your toes and going up to your head. Doing this may help your symptoms.
When to call for help during self-care
Call a doctor if any of the following occur during self-care at home:
- New or worse signs of infection, such as warmth, redness, swelling, pus, or a fever.
- Symptoms occur more often or are more severe.
Learn more
Over-the-counter medicines
More self-care
Current as of: November 16, 2023
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: November 16, 2023
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
This information does not replace the advice of a doctor. Ignite Healthwise, LLC, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.