What is pulmonary stenosis?
Pulmonary stenosis is relatively common and accounts for about 10% of heart defects diagnosed during childhood. It can occur in children with otherwise normal hearts or along with other congenital heart defects such as atrial septal defect or Tetralogy of Fallot. It occurs more frequently in children with Noonan syndrome and Williams syndrome which are both rare genetic conditions.
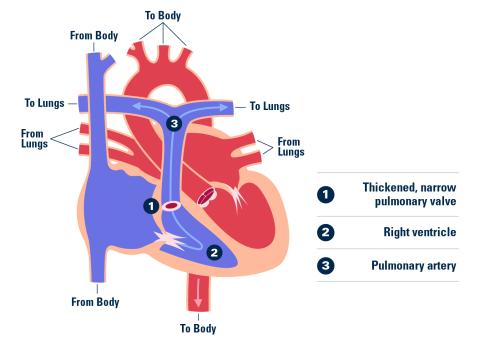
The heart is a four-chambered pump with four heart valves. The valves are made of thin flaps of tissue that open to allow the blood to flow forward and close to prevent the blood from flowing backwards. The pulmonary valve (1) is located on the heart's right side. Blue blood that comes from the body is pumped from the right lower chamber called the right ventricle (2) to the pulmonary artery (3) and then circulates to the lungs.
When a child has pulmonary stenosis, the area where blood exits the heart's lower right chamber is too narrow. Usually, the pulmonary valve itself is affected which is called valvar pulmonary stenosis. This problem is often caused by fusion of the valve leaflets. Subvalvar stenosis is the term used when the narrowed area is below the valve. Supravalvar stenosis is the term used when the narrowed area is above the valve.
What are the effects of this problem on my child's health?
The health effects of pulmonary stenosis are related to the severity of the narrowing and the presence of other heart defects. The severity of narrowing is measured as the pressure difference across the affected area. The higher the number, the greater degree of narrowing and the harder the right heart has to work to pump blood to the lungs. Mild pulmonary stenosis is when the pressure difference is less than 30-40 mmHg, moderate pulmonary stenosis is when the pressure is 40 to 60 mmHg, and severe pulmonary stenosis is when the pressure is greater than 60-70 mmHg. Critical pulmonary stenosis is a term used in infants born with very severe narrowing (greater than 90 mmHg) and requires treatment soon after birth.
Mild pulmonary stenosis is not expected to have any short or long term health effects and rarely gets more severe over time. Moderate to severe pulmonary stenosis increases the workload of the heart's right side and can eventually cause damage to the heart muscle. This can result in symptoms of shortness of breath with exercise and low stamina. If left untreated, eventually the heart muscle weakens and symptoms of right-sided heart failure may develop.
In a baby born with critical pulmonary stenosis, the opening is so small that the heart cannot pump enough blood to meet the baby's needs. Unless the problem is treated early, the baby will develop problems due to right-sided heart failure.
Children with pulmonary stenosis are at increased risk for subacute bacterial endocarditis (SBE). This is an infection of the heart caused by bacteria in the blood stream. It most commonly occurs after a dental or other medical procedure and can usually be prevented by a dose of antibiotic prior to the procedure.
Exercise recommendations: Exercise recommendations are best made by a patient's doctor so that all relevant factors can be included in the decision. There usually are no restrictions placed on patients with pulmonary stenosis who have <40mmHg gradient and an otherwise normal heart. Patients who achieve a good result with catheter or surgical dilation of the narrowing are usually not restricted from any physical activities.
How is this problem diagnosed?
Clinical features: Symptoms are related to the degree of narrowing and usually develop slowly over time. Possible symptoms include shortness of breath with exercise and low stamina. Critical pulmonary stenosis in the newborn can cause blueness of the lips (a condition called cyanosis) and/or congestive heart failure.
Physical findings: The diagnosis is most often made due to the presence of a heart murmur. The loudness of the murmur is helpful in predicting the degree of narrowing. Loud murmurs usually suggest that there is at least a moderate degree of narrowing. Growth and development is expected to be normal unless there are other health problems.
Medical tests: In patients with moderate to severe pulmonary stenosis, the electrocardiogramoften shows increased right ventricular forces (overdevelopment of the right heart muscle). The chest xray is most often normal. An echocardiogram is able to detect even minor degrees of pulmonary stenosis with almost 100% accuracy. Cardiac catheterization is rarely needed for diagnostic purposes but balloon angioplasty during heart catheterization is often done to treat the problem.
How is the problem treated?
Treatment options for pulmonary stenosis include open-heart surgery or balloon angioplasty. The primary indication for treatment is the degree of narrowing and treatment is timed to prevent damage to the right heart.
Balloon angioplasty Balloon angioplasty has proven to be an excellent treatment option for children with pulmonary stenosis. This procedure is done in the heart catheterization laboratory and avoids the need for surgery. During the procedure catheters (thin plastic tubes) are placed into the large blood vessels in the legs and gently guided to the heart. The catheter tip is placed across the pulmonary valve and the balloon tip is inflated. The balloon gently dilates the narrowed area. This procedure achieves a good result in most patients and no further treatment is ever needed. Patients with Noonan and Williams syndromes and patients with a very small pulmonary valve are less likely to achieve good results from the procedure.
Some degree of leakage from the pulmonary valve is not uncommon after this procedure. It is usually mild, well tolerated, and does not require any treatment. Other problems stemming from the procedure are uncommon but can include bleeding, infection, and perforation of the heart with the catheters.
This procedure is done with IV sedation and usually the patient can go home the following day.
Surgical valvotomy Another treatment option for patients with severe pulmonary stenosis is direct incision of the fused leaflets of the valve during open-heart surgery. During this procedure an incision, called a midline sternotomy, is made down the middle of the chest. A heart lung machine is used to support the patient while the heart is opened and the pulmonary valve is repaired. Surgical repair is preferred when there is more extensive narrowing in addition to the pulmonary valve itself, often as a result of narrowing below and/or above the valve. In these situations, a patch may be needed to enlarge narrowed areas in addition to valve repair. The results from this procedure are also excellent. Hospital length of stay is short (3 or 4 days) and complications are rare. Mild residual narrowing is common but will not result in long-term problems. Valve leakage may also occur but is very well tolerated without the need for valve replacement.
Clinics
Care and services for patients with this problem are provided in the Congenital Heart and Cardiovascular Surgery clinics at the University of Michigan Medical Center in Ann Arbor.
What is the outlook for children with this diagnosis?
Overall, the outlook for children with this diagnosis is excellent.
References
Cheatham JP. Pulmonary stenosis. In Garson A, Bridker JT, McNamr DG (Eds): The Science and Practice of Pediatric Cardiology, Vol I, Philadelphia PA: Lea & Febiger: 1997; 1207-1256.
Rome JJ. Balloon pulmonary valvuloplasty. Pediatr Cardiol 19:1998;18-24.
Rowland TW. Congenital obstructive and valvular heart disease. In B Goldberg (Ed) Sports and exercise for children with chronic health conditions. Champaign IL: Human Kinetics 1995, 232-233.
Written by: S. LeRoy RN, MSN
Reviewed September, 2012
